Wouldn’t it be great if someone got a second chance in life with a single medical procedure? That’s the miracle a stem cell transplant can do, if done properly. A stem cell transplant replaces unhealthy bone marrow with healthy stem cells. The healthy and powerful cells regenerate the blood and immune system. Moreover, they produce new blood cells, assist the body in fighting infections, and help re-energize the body.
The transplants help many patients with blood cancers, rare blood disorders, or a weak immune system. It is not just treatment; it is often the only hope for recovery. In this article, we’ll explain everything about stem cell and bone marrow transplants in simple words. It includes the types, diseases they treat, how they work, side effects, risks, and costs. Let’s dig in.
What is Stem Cell or Bone Marrow Transplant?
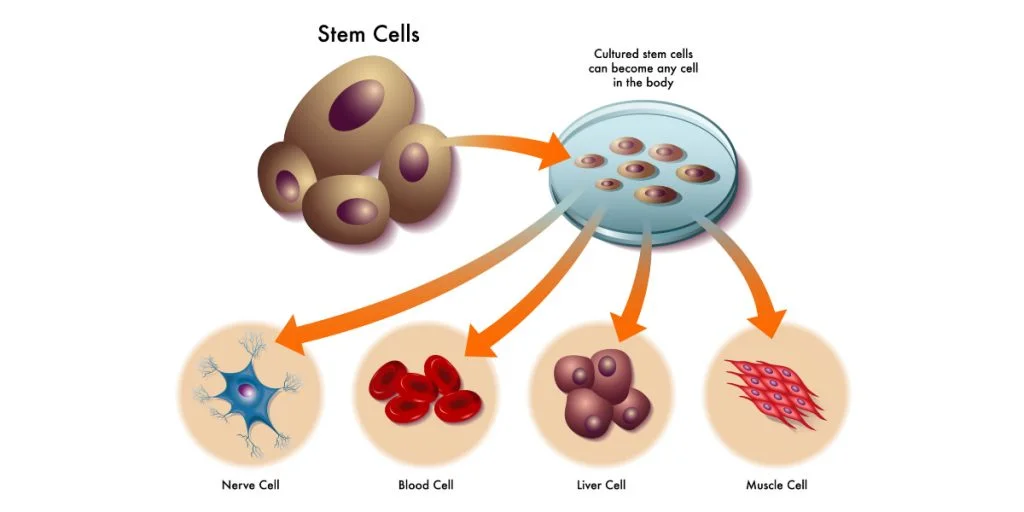
Stem cells are unique cells that can change into different types of blood cells. They make red blood cells to carry oxygen, white blood cells to combat infections, and platelets to stop bleeding. The body cannot survive without sufficient healthy stem cells. A transplant is a treatment procedure that provides the body with new and healthy stem cells. These are new cells that are used to replace the damaged or destroyed bone marrow. Gradually, they regenerate the blood and the immune system.
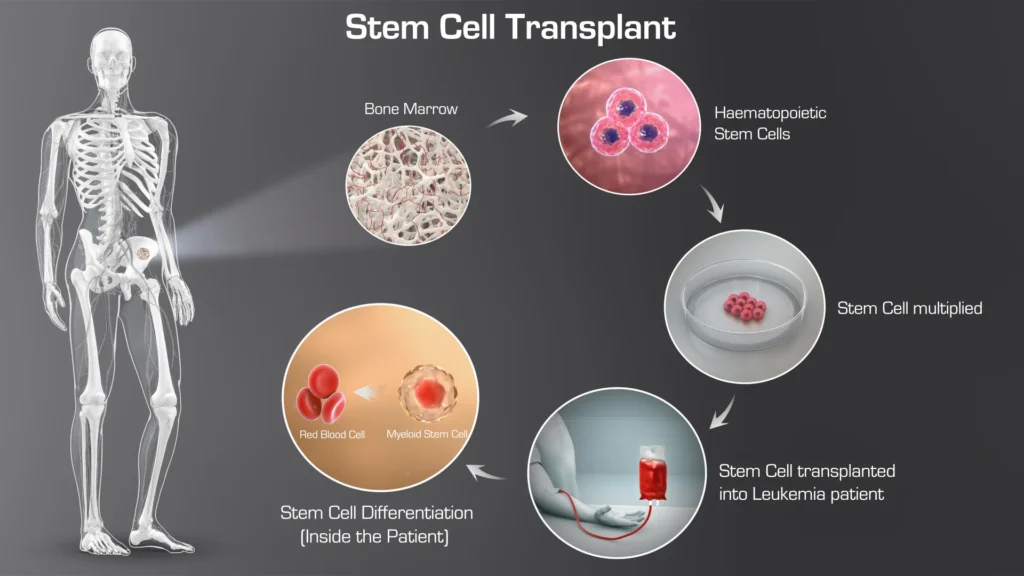
A bone marrow transplant is one of the types of stem cell transplants. Previously, doctors relied primarily on the bone marrow stem cells. They can even gather the stem cells in the blood or cord blood today. That is why you can hear both terms. Therefore, we can agree that bone marrow and stem cell transplants are life-saving procedures. They can heal where other treatments fail.
Types of Stem Cell Transplant
Every transplant is different. Doctors choose the type based on the patient’s health, the disease, and the source of the healthy stem cells.
The main types of treatments are
- Autologous Transplant
- Allogeneic Transplant
- Syngeneic Transplant
- Cord Blood Transplant
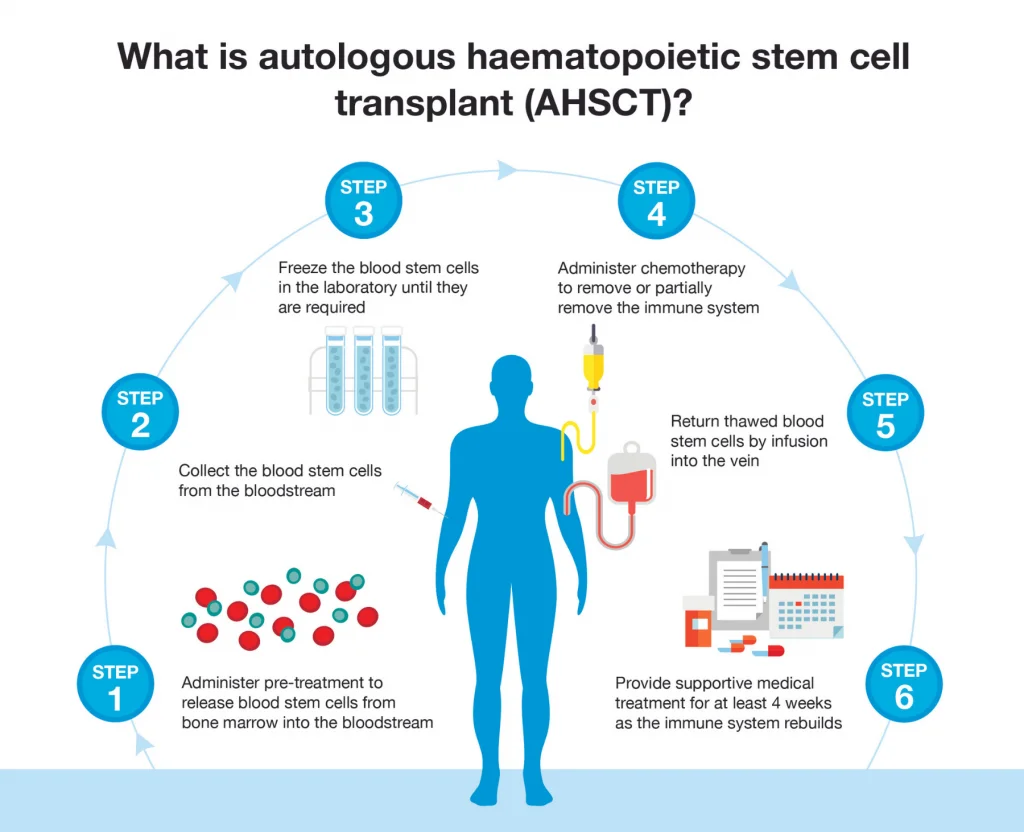
Autologous Transplant
Here, doctors use the patient’s own stem cells. They collect them before strong treatments like chemotherapy, then return them afterward. This type lowers the risk of rejection because the body already knows its own cells.
Allogeneic Transplant
For this kind of stem cell transplant, stem cells come from a donor, who is usually a brother, sister, or someone who is not related but is a good match. There’s a chance that the body will reject the new cells because they are not from the body. That is why it is so important to match.
Syngeneic Transplant
This happens when the donor is an identical twin. Since the genetic match is perfect, it reduces many risks. But of course, not many people have this option.
Cord Blood Transplant
These stem cells originate from blood taken from the umbilical cord at birth. There are fewer cells, but they can still grow well in the body. This option is especially useful when finding a close donor match is hard.
Diseases Treated by Stem Cell and Bone Marrow Transplants
Stem cell and bone marrow transplants are not just for one simple illness. Doctors use stem cells for many serious conditions where the bone marrow cannot make healthy blood cells anymore.
The most commonly treated diseases are:
Blood Cancers
Leukemia, Lymphoma, Myelodysplastic syndromes (MDS), and Multiple Myeloma are all conditions that doctors often treat with transplants. These types of cancer damage the blood cells and the bone marrow. A transplant helps put healthy ones in their place.
Blood Disorders
The body can’t make regular blood cells when someone has Aplastic anemia, an autoimmune disease, a genetic or acquired problem, sickle cell disease (SCD), or thalassemia. Stem cell transplants can get the output back to normal and make life better.
Immune System Problems
Some people are born with weak immune systems that can’t protect them from getting sick. The body can get a new immune system after a donation that works better to protect it.
Rare Diseases
Sometimes, stem cell transplants can also help treat genetic or metabolic diseases. These happen less often, but when they do, they can change your life.
Stem Cell and Bone Marrow Transplant Procedure: Step by Step
A stem cell transplant is not an easy process. It happens in stages, and each step matters for the treatment to succeed.
- Collecting Stem Cells
- Conditioning Treatment
- Infusion of Stem Cells
- Engraftment Phase
- Recovery in Hospital
Step 01: Collecting Stem Cells
The first step is gathering healthy stem cells. They may come from the patient, a donor, or cord blood. Doctors use special machines to collect stem cells from blood, or in some cases, directly from bone marrow.
Step 02: Conditioning Treatment
Before the transplant, the patient usually receives chemotherapy, sometimes with radiation. This clears out the diseased bone marrow and makes space for the new stem cells to grow. It also helps weaken the disease.
Step 03: Infusion of Stem Cells
Next comes the actual transplant. The collected stem cells are given through a vein, much like a blood transfusion. This part is usually painless and takes only a few hours.
Step 04: Engraftment Phase
After the infusion, the stem cells travel to the bone marrow and begin to grow. This stage is called engraftment. It can take two to six weeks. During this time, doctors check the patient closely for infections and complications.
Step 05: Recovery in Hospital
The patient often stays in the hospital until the new stem cells start making enough healthy blood cells. Supportive care, like antibiotics, nutrition, and blood transfusions, helps the body stay strong.
Side Effects and Risks of Stem Cell and Bone Marrow Transplants
Like any major medical treatment, stem cell and bone marrow transplants come with side effects. But effects vary from patient to patient. Knowing them helps patients and families prepare.
Short-Term Side Effects
These usually happen in the first few weeks after the transplant:
- Fatigue and weakness
- Nausea, vomiting, or diarrhea
- Low blood counts, leading to infections or bleeding
- Mouth sores or loss of appetite
- Hair loss due to chemotherapy
Doctors monitor patients closely and give medicines or support to reduce these effects.
Long-Term Risks
Some complications can appear months or even years later:
- Graft-versus-host disease (GVHD): When donor cells attack the patient’s body
- Organ problems, like liver or lung issues
- Infertility or hormonal changes
- Weakened immunity, making infections more likely
- Rarely, relapse of the original disease
Managing Side Effects
Regular check-ups, medications, healthy nutrition, and careful hygiene help manage side effects. Emotional support and counseling are also important for faster recovery. While the risks are real, many patients recover well and regain a normal life, especially with close monitoring and care.
Success Rate and Outcomes of Stem Cell Transplants
Many people wonder: how likely is a stem cell transplant to work? The answer depends on several factors, but it can be life-changing for many patients.
For measuring success, doctors look at:
- Survival rates: How long patients live after the transplant
- Remission rates: Whether the disease comes back
- Quality of life: How well patients recover physically and emotionally
Factors That Affect Success
- Type of disease: Blood cancers often have higher success rates than other disorders
- Age and overall health: Younger, healthier patients usually recover faster
- Donor match: A close match between donor and patient improves outcomes
- Type of transplant: Autologous, allogeneic, syngeneic, or cord blood — each has different risks and benefits.
General Insights
Survival rates vary by illness and type of transplant around the world. Every year, new drugs and better care make things better for many people who go into recovery.
A stem cell or bone marrow transplant isn’t a guarantee to get better. But it can give people hope when other methods don’t work. Patients can often get stronger and go back to their normal lives with careful care and tracking.
Cost of Stem Cell and Bone Marrow Transplants
Stem cell and bone marrow transplants are complex treatments, and costs can vary widely. Several factors influence the total expense.
Factors Influencing the Cost:
1. Type of Transplant
Autologous transplants (using the patient’s own stem cells) are usually less expensive. Allogeneic transplants (using donor cells) tend to cost more due to donor matching and additional care.
2. Hospital and Location
Treatment costs vary by hospital, country, and city. Private hospitals and advanced centers typically charge higher fees than public or regional hospitals.
3. Donor Matching
Finding a compatible donor, especially for unrelated allogeneic transplants, can increase costs because of testing, travel and logistics.
4. Pre- and Post-Transplant Care
Expenses include chemotherapy or radiation before the transplant, hospital stay, medications, follow-ups, and monitoring for complications.
5. Patient-Specific Factors
Age, overall health, and disease severity can affect treatment complexity and length of hospitalization, which adds to the cost.
Conclusion
Stem cell and bone marrow transplants can change a person’s life and give them real hope if they have a dangerous blood disease or cancer. They can get the body’s ability to fight off sickness and heal itself back by swapping sick cells with healthy ones. Yes, the procedure is complex, and the journey can feel overwhelming. But patients and their families can see the way more clearly if they know the steps, types of donations, possible side effects, success rates, and costs.
If you want to get a stem cell transplant, talk to a medical team you can trust. As you go through treatment, they can talk you through each step and answer any questions you have. Last but not least, a stem cell transplant is more than just a medical process. Many people see it as a sign of power, resilience, and the chance of a healthy future.